Exercise improves symptoms and function for people with ankylosing spondylitis
Why was this study needed?
Ankylosing spondylitis affects around 200,000 people in the UK, mostly starting before the age of 45. People with ankylosing spondylitis may have difficulty with everyday activities and with work. There is no cure, but there are some approaches to manage symptoms including medication, physiotherapy, exercise and sometimes surgery.
Although exercise has long been recommended for people with ankylosing spondylitis, few studies have properly tested how effective it is. Meanwhile, drug treatments have changed a lot in recent years, with new drugs that suppress the immune system (called anti-TNFs) being introduced. It is unclear whether these new therapies have altered the benefit of carrying out exercise.
Ankylosing spondylitis affects around 200,000 people on the UK, mostly starting before the age of 45
This study looked at a range of exercise programmes, and also examined whether exercise had a lesser or greater benefit in studies that included people receiving anti-TNF drugs.
What did this study do?
This systematic review identified eight randomised controlled trials evaluating exercise in 331 people with ankylosing spondylitis. All participants were diagnosed according to one of two sets of standard criteria (Assessment of SpondyloArthritis International Society or modified New York criteria) though disease duration and severity varied.
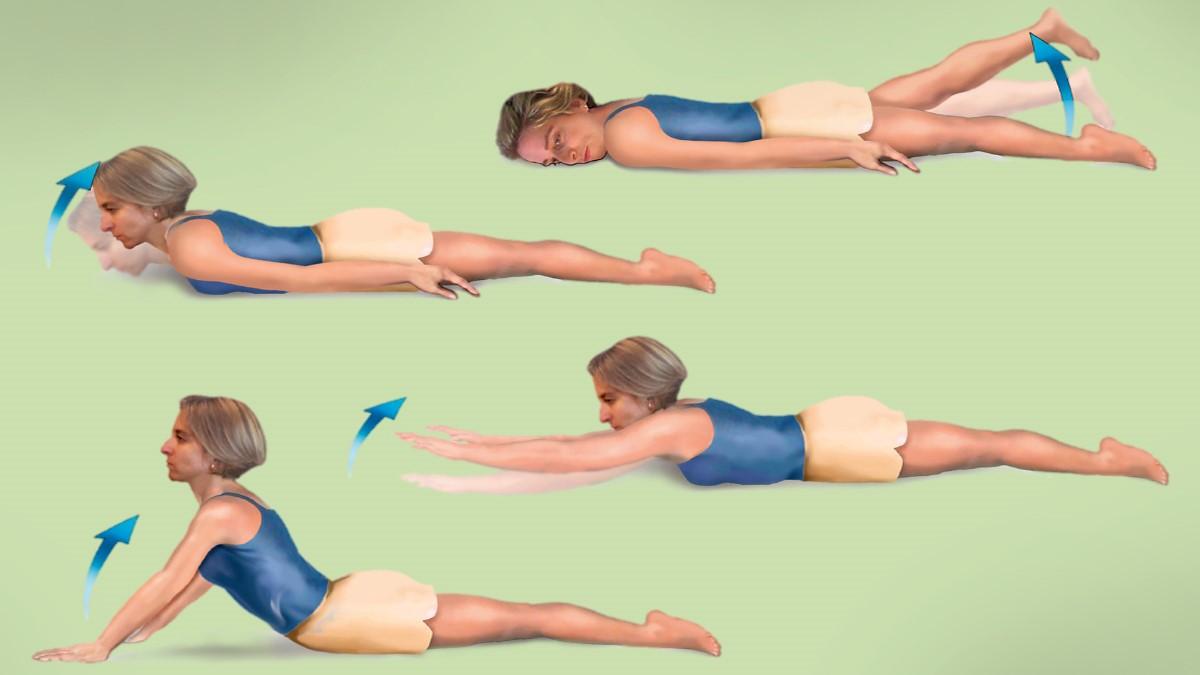
Interventions included home-based exercise, swimming and Pilates compared with usual care, education or physical therapy in one study. Programmes lasted from three to 12 weeks.
Studies provided data on two validated 10-point outcome scales: the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) for measuring symptoms, and the Functional Index (BASFI) to look at day-to-day activities. Four of the eight studies came from Turkey, two Norway, one Spain and one Italy. All took place after 2005. Studies were pooled in meta-analysis regardless of intervention type.
What did it find?
Exercise improved symptoms on the BASDAI scale. Exercise groups scored on average 0.90 points lower than control groups (95 percent
confidence interval [CI] -1.52 to -0.27) in a meta-analysis of all eight studies. This result is a weighted mean difference (WMD) which takes greater account of larger studies. There was considerable difference in results (heterogeneity) between individual studies.
Exercise also improved day-to-day function on the BASFI scale (WMD -0.72, 95 percent CI -1.03 to -0.40) with no heterogeneity between the
eight studies for this outcome.
Exercise gave apparently greater benefit when limited to the four studies that included people who received anti-TNF therapies. Symptoms
improved by WMD -1.37 (95 percent CI -1.90 to -0.84) on the BASDAI, and daily activities by WMD -0.81 (95 percent CI -1.25 to -0.38) on the
BASFI. Findings were similar across all four studies.
What does current guidance say?
NICE produced recent guidelines (2017) on the management of spondyloarthritis, which includes ankylosing spondylitis and other inflammatory arthritis such as psoriatic arthritis.
NICE recommends that people with spondyloarthritis affecting the spine should be referred to a specialist physiotherapist to start an individualised, structured exercise programme. This should include deep breathing and aerobic exercise, stretching, strengthening and postural exercises, spinal extension and a range of motion exercises for the spine.
Exercise and stretching are also emphasised as a component of self-care during disease flare-ups.
What are the implications?
The findings show that exercise yields measurable improvements in symptoms and physical function scores. The results broadly support the current NICE guidelines that exercise should be a core component of care in people with ankylosing spondylitis.
It would be nice to know more about how this exercise should be carried out – for example, at home or in a supervised group. By analysing all types of exercise programme together, it is not possible to tell if some types of exercise are more effective than others.
Citation and Funding
Pécourneau, V, Degboé, Y, Barnetche, T, et al. Effectiveness of exercise programs in ankylosing spondylitis: a meta-analysis of randomised controlled trials. Arch Phys Med Rehabil. 2017. [Epub ahead of print]. This study did not report any funding.
The full NIHR Signal and additional expert commentary was published on 21 November 2017.
Commentary
Will Gregory, in collaboration with the AStretch committee
Terminology for this condition is changing and ankylosing spondylitis is now being referred to as the broader axial spondyloarthritis (AxSpA). Whatever we call it, it is still hard to spell – and harder to live with, often having a significant impact on daily activities.
It is fantastic that this review confirms the long-held beliefs about the benefits of exercise, both on functional outcomes and controlling the symptoms of AxSpA. Most people present with the condition in their 20s and, with a full life ahead and gainful employment to maintain, keeping fit and active are vitally important. The condition affects many joints of the body as well as the skin, eyes, bowel and connective tissue. As well as these, there are cardiovascular and osteoporosis risks. These body-wide effects can be hard to manage and have a debilitating impact.
For many, new drugs help. However, in regularly working with people with AxSpA, we see that exercise can vastly improve our patients’ outcomes and well-being. Once taught, exercise can be done with ongoing supervision and review, at home or in a pool. But research (Derakhshan et al 2018) shows that access to appropriately trained healthcare professionals and specialist services is patchy. Hydrotherapy pools are also often under threat. We need to ensure access across the UK.
AStretch is a not for profit organisation which provides a co-ordinated approach to the planning and delivery of education and best practice. AStretch also supports physiotherapists working with people who have AxSpA. Twitter @AStretch_Physio
- Will Gregory is acting consultant physiotherapist (rheumatology) Salford Royal Hospital and an AStretch committee member
Number of subscribers: 2